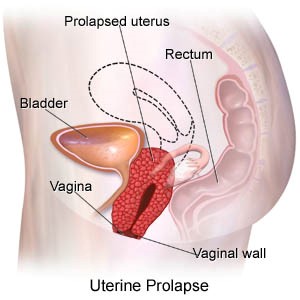
You have a baby or two, and think nothing more about your uterus – until it starts bulging out of your vagina. Or you navigate your way through menopause, relieved when it is over – only to find that your bladder has fallen down and become bothersome.
A woman’s pelvic area contains numerous organs – including the bladder, uterus, vagina and rectum. Each has a very different function, but all are held in place by the muscles and connective tissue of the pelvic floor. When one prolapses, it can affect the others.
Pelvic organ prolapse is the downward bulging of one or more of the pelvic organs into the vagina. It is extremely common, and results in everything from mild discomfort to bothersome vaginal bulge symptoms.
Causes and Symptoms of Pelvic Organ Prolapse
Evaluating Pelvic Organ Prolapse
Types of Pelvic Organ Prolapse
Non-surgical Treatments for Pelvic Organ Prolapse
Pelvic Organ Prolapse Surgery
Why Virginia Mason?
Several of our pelvic floor specialists have advanced training, and are board-certified in Female Pelvic Medicine and Reconstructive Surgery. They have the experience and expertise to address complications of prior surgeries, recurrent prolapse, or complex pelvic floor problems. We are committed to making sure you are fully informed about all your choices, and partner with you to improve your pelvic health.
Causes and Symptoms of Pelvic Organ Prolapse
Pelvic organ prolapse occurs when the pelvic muscles become weak or injured. The most common cause of pelvic organ prolapse is childbearing. During childbirth, the support structures become weakened and eventually no longer hold organs in their proper places.
Menopause can also contribute to pelvic organ prolapse as hormone levels decrease and tissues become more lax.
Other common causes include:
- Tobacco use
- Prior pelvic surgery, including hysterectomy
- Family history
- Obesity
- Chronic cough
- Constipation
The most common symptoms of pelvic organ prolapse include:
- Vaginal pressure that worsens with standing, coughing or as the day progresses
- Feeling of heaviness or fullness in the pelvic area
- Sensation of a bulge or “ball” protruding through the vaginal opening
Evaluating Pelvic Organ Prolapse
At Virginia Mason, our comprehensive evaluation includes a complete medical history and physical exam. Other tests to help determine the best treatment option may include:
- Cystoscopy, which looks inside the bladder and urethra with a tiny camera
- Urodynamic testing in our lab to evaluate how the bladder and urethra are working
Types of Pelvic Organ Prolapse
Normal pelvic support looks like this:
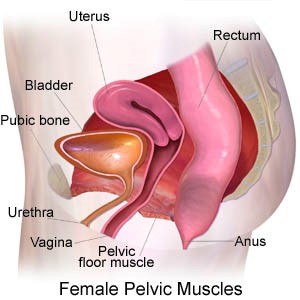
There are three primary types of pelvic organ prolapse. All descend into the vagina, and you may have more than one type of prolapse.
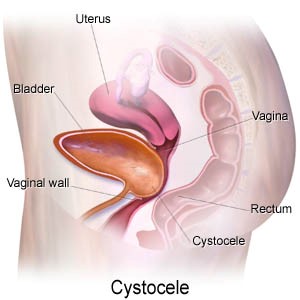
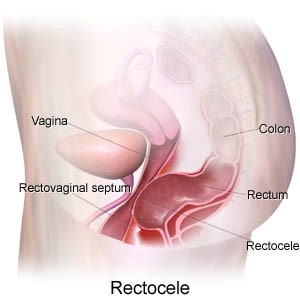
The top of the vagina can also prolapse through the vagina, which is called vaginal vault prolapse. This can happen after a hysterectomy. If the bowels are prolapsing, it is called an enterocele.
Non-surgical Treatments for Pelvic Organ Prolapse
There are various treatment options available for pelvic organ prolapse.
Treatments include:
- Pelvic floor muscle strengthening, called Kegel exercises
- Pelvic floor physical therapy, with a program created specifically for you
- Supplemental vaginal estrogen to help restore vaginal tissues
- A vaginal pessary (a small, removable device) that supports the vagina and keeps the prolapse inside
Lifestyle changes include stopping smoking and losing weight. Even modest amounts of weight loss can improve your condition.
Pelvic Organ Prolapse Surgery
When non-surgical treatments do not help with pelvic organ prolapse, surgical options are available to restore vaginal support and improve pressure or bulging.
For bladder or rectal prolapse, surgical repair can be done using a variety of techniques, including:
- Native tissue repair, which is a surgical repair using your own tissue
- A biological graft, a surgical repair in which a graft material is used to strengthen the repair
- Abdominally placed lightweight polypropylene mesh placed during sacrocolpopexy surgery
At Virginia Mason, transvaginal mesh – large supportive pieces of polypropylene mesh placed through the vagina – is not typically done because of the problems associated with it.
For uterine prolapse or vaginal vault prolapse, the surgical approach depends on the severity of the prolapse, and other factors. Some procedures are done through the vagina, others through the abdomen.
Abdominal repairs may be performed through an open incision, or robotically with laparoscopy. With a vaginal approach, ligaments in the pelvis are used to re-support the top of the vagina.
A common procedure called sacrocolpopexy involves attaching a piece of mesh to the vagina and the ligaments on the tailbone. It can be performed with laparoscopy, robotically, or through an open abdominal incision.
Surgery for stress urinary incontinence and pelvic organ prolapse can be performed at the same time, if necessary. Some women also need a hysterectomy at the same time prolapse repair is done.
Why Virginia Mason?
When it comes to treating this intimate part of the body, you want experts with a history of great outcomes. Our view is that this is a complicated part of the body, where the whole system needs to be taken into consideration – including urinary function, bowel function, and the ability to have and enjoy sex.
Virginia Mason is one of the largest referral centers in the area for pelvic floor issues. Physicians throughout the Pacific Northwest region and Alaska refer their patients to us because our gynecologists, urogynecologists and urologists are renowned experts in pelvic organ prolapse repair.
Several of our pelvic floor specialists have advanced training, and are board-certified in Female Pelvic Medicine and Reconstructive Surgery. They have the experience and expertise to address complications of prior surgeries, recurrent prolapse, or complex pelvic floor problems.
We are committed to making sure you are fully informed about all your choices, and partner with you to improve your pelvic health.